
Gynecomastia Surgery
Detailed Procedure Information
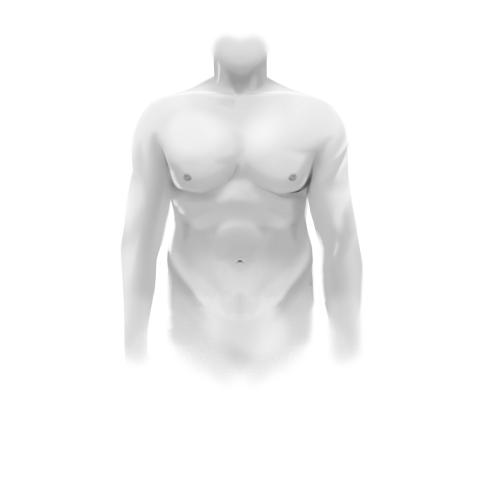
Gynecomastia surgery, often termed male breast reduction or reduction mammaplasty for men, is designed to address the condition of enlarged male breasts. This specialized procedure refines the chest contour by removing excess glandular tissue, fat, and skin, resulting in a more masculine and natural-looking chest profile.
Understanding Gynecomastia Surgery
Men who experience discomfort or dissatisfaction with the size and appearance of their chest may find gynecomastia surgery a valuable solution. This procedure is suitable for those who have tried non-surgical options such as weight loss and exercise but have not achieved the desired chest contour.
Who Should Consider Gynecomastia Surgery?
- Men unhappy with enlarged breasts, nipples, or areolas.
- Those experiencing physical discomfort or self-consciousness due to breast size.
- Individuals who want a permanent correction after diet and exercise have failed.
- Those wishing to improve body proportion and self-esteem.
Benefits of Male Breast Reduction
- Reduction of excess breast tissue for a flatter chest.
- Improved symmetry and chest contour.
- Correction of disproportionately large or misshaped nipples and areolas.
- Physical relief from discomfort associated with gynecomastia.
- Long-lasting, natural-looking results that enhance confidence.
- Comfort when wearing fitted clothing or appearing shirtless.

Preoperative Considerations
Consultation with a board-certified aesthetic plastic surgeon is essential before surgery. Key points to consider include:
- Overall good health and absence of untreated medical conditions.
- Ruling out rare medical causes with your primary care physician before surgery.
- Distinguishing between true glandular gynecomastia and pseudogynecomastia (fatty chest tissue), as the latter may respond well to non-surgical approaches or liposuction alone.
- Skin quality and elasticity, which may affect surgical technique and outcomes — poorer elasticity can result in looser skin post-procedure.
- Achieving a healthy body weight close to your ideal before surgery for optimal results.
- Avoidance of substances such as marijuana, steroids, and excessive alcohol, which may contribute to gynecomastia.
- Understanding the possibility of visible scarring and managing expectations about the final result.
- Commitment to maintaining stable weight post-surgery for lasting contour.
- Anticipation of a recovery period that typically lasts one to two weeks, depending on procedure extent.
Selecting a Surgeon
Choosing a qualified and experienced surgeon is crucial for successful gynecomastia surgery. Consider these factors when selecting your plastic surgeon:
- Verify the surgeon’s credentials, board certification, and specialized training in aesthetic plastic surgery.
- Ensure the surgeon has extensive experience with male breast reduction procedures.
- Review before and after photographs of previous gynecomastia patients to assess surgical outcomes.
- Consider your comfort and rapport with the surgeon during initial consultation.
- Look for membership in reputable professional organizations such as The Aesthetic Society.
What to Expect During Your Consultation
During your initial consultation, you and your surgeon will review your goals and medical history. The surgeon will perform a thorough physical examination of your chest to evaluate:
- Current breast size, shape, and tissue composition.
- Skin quality and elasticity.
- Positioning and size of nipples and areolas.
- Overall health and suitability for surgery.
Be prepared to discuss:
- Previous surgeries or medical conditions.
- Medications, allergies, and lifestyle factors including tobacco, alcohol, and recreational drug use.
- Your history with any prior cosmetic or noninvasive procedures.
Pertinent Questions to Ask Your Surgeon
- Am I an appropriate candidate for gynecomastia surgery?
- What are realistic expectations for my results?
- Can you show me photos of similar cases?
- How many gynecomastia surgeries have you performed?
- What surgical techniques will you use?
- Where will the procedure be performed and how long will it take?
- What type of anesthesia is recommended?
- What postoperative scars should I expect?
- What is the estimated recovery time?
- What risks and complications should I be aware of?
- Are revision procedures an option if I am unsatisfied?
Post-Consultation Guidance
After your consultation, your surgeon will provide tailored recommendations regarding surgical approach, likely outcomes, anesthesia options, recovery timeline, and associated costs. If uncertain, you are encouraged to seek a second opinion or ask additional questions to ensure an informed decision.
Preparing for your Procedure
Proper preparation before gynecomastia surgery contributes significantly to the success and safety of your procedure. Your surgeon will provide specific preoperative instructions, which typically include:
- Completing a comprehensive medical evaluation including any necessary laboratory tests and medical clearances.
- Achieving a stable, healthy weight and lifestyle modifications such as smoking cessation to optimize healing.
- Discontinuing medications and supplements that may increase bleeding risk, including aspirin, NSAIDs, vitamin E, and certain herbal supplements. Your surgeon will advise on exact timelines for stopping these substances.
- Hydrating well before and after surgery to promote recovery.
- Avoiding sun exposure and tanning of chest skin for at least two weeks prior to surgery to reduce scar risk.
- Not shaving or waxing the chest area two weeks before and six weeks after surgery to minimize skin irritation.
- Notifying your surgeon promptly if you develop any infections, colds, or illnesses in the week leading up to surgery.
- Arranging for adequate time off work—typically about one week, longer if you have physically demanding work.
- Preparing your home for recovery by setting up easy access to necessities, entertainment, medications, and meals to allow for restful healing.
- Ensuring transportation arrangements for the day of surgery and the first night post-operation, as you will not be able to drive.
The Day of Surgery
Your gynecomastia surgery will be performed in an accredited surgical facility, which might be a hospital, ambulatory center, or specialized surgical suite. Typical aspects include:
- Duration of the procedure usually ranges from one to three hours, variable by technique and complexity.
- General anesthesia is most commonly used, although local anesthesia with sedation may be appropriate in certain cases.
- Continuous monitoring of vital signs during surgery to ensure safety.
- Application of a compression garment immediately post-operation to support the new chest contour.
- Occasional use of surgical drains depending on surgical extent, discussed beforehand with your surgeon.
- Postoperative monitoring in a recovery area prior to discharge home.
Aftercare & Recovery
Recovery from gynecomastia surgery varies depending on individual factors and surgical complexity. Typically, patients can expect to resume work within one week when the procedure involves liposuction combined with tissue excision. Your surgeon will customize your postoperative care instructions.
Initial Postoperative Period
- Compression garments or bandages will be worn continuously to minimize swelling and support healing.
- Mild to moderate discomfort is common once anesthesia wears off; your surgeon may prescribe pain control medication or recommend over-the-counter options.
- Redness, bruising, and swelling are expected and will gradually subside over several weeks.
- Avoid activities that increase blood pressure or strain the chest area, including heavy lifting, bending, or vigorous arm movement, during the initial days.
- Rest is critical, with limited upper body movement particularly in the first three days following surgery.
Follow-Up and Healing Timeline
- Your first postoperative visit generally occurs within five to seven days to assess healing, remove sutures or drains if placed, and evaluate the surgical sites.
- Duration of compression garment use will be directed by your surgeon, often spanning several weeks to optimize contour.
- Sensation changes around the nipples or chest area are normal and typically improve within months to a year.
- Swelling may persist and diminish progressively over three months or longer.
- Patients are encouraged to avoid sun exposure on healing scars for approximately six weeks to reduce discoloration and improve scar appearance.
- Gradual resumption of low-impact exercise can begin at about two to three weeks post-surgery, with progressive upper body strengthening exercises introduced cautiously between three to six weeks as advised by your surgeon.
Individual recovery experiences vary, so maintaining communication with your surgeon and adhering to aftercare guidelines is vital.
Results
Longevity of Results
The reshaped chest contour achieved through gynecomastia surgery generally endures long-term, provided your weight remains stable. Recurrence may happen if the underlying cause of enlarged breasts, such as certain medications or anabolic steroid use, continues or returns.
Expected Outcomes
Patients frequently report improved body proportion, enhanced self-confidence, and satisfaction with their appearance following surgery. Viewing before and after photo galleries can help set realistic expectations and provide insight into typical outcomes.
Postoperative Considerations
Ongoing follow-up appointments allow your surgeon to monitor healing and address any concerns. Promptly reporting any unexpected changes or issues supports the best possible final result.
Incisions and Scars
Incision Techniques
The type and location of incisions used in gynecomastia surgery depend on individual patient anatomy, severity of tissue enlargement, and the specific surgical approach chosen. The primary methods include:
Liposuction
Small, discreet incisions are made in concealed locations on the chest to insert the cannula for fat removal. These incisions are typically minimal, leaving tiny scars.
Excisional Surgery
When removal of glandular tissue is necessary, an intra-areolar (Webster) incision is made along the lower half of the areola’s border. In cases requiring reduction of areola size, the incision extends circumferentially around the entire areola.

Combination of Liposuction and Excision
Most patients require a combination approach involving liposuction incisions and an areolar incision to effectively contour the chest and eliminate glandular tissue. Severe cases may also warrant skin excision or nipple repositioning.
Scar Expectations
The extent and visibility of scars after gynecomastia surgery vary:
- Minimal fat-only gynecomastia typically results in very small scars hidden in natural creases.
- Significant glandular tissue removal usually leaves scars along the areolar border.
- Areolar size reduction scars encircle the nipple and can be more noticeable initially.
- Patients with large, female-type breasts may have additional scarring concealed in chest folds.
While these scars are permanent, most fade considerably over time. Expert surgical technique focusing on precise tissue handling and suture methods minimizes scar prominence. Proper postoperative care and protection from sun exposure are also essential for optimal scar maturation.
Safety Considerations
Risk and Complications
Although gynecomastia surgery is generally safe, it carries inherent surgical risks. It is critical to discuss these with your surgeon during consultation to understand your personalized risk profile.
General surgical risks include:
- Adverse reactions to anesthesia.
- Hematoma or seroma formation, which may require drainage.
- Infection or bleeding at the surgical site.
- Changes or loss of sensation, typically temporary but occasionally persistent.
- Visible scarring or abnormal scar formation.
- Allergic reactions to medications or materials used during surgery.
- Damage to underlying tissues or structures, though rare.
- Unsatisfactory cosmetic results requiring revision procedures.
Specific gynecomastia surgery risks also include:
- Deep vein thrombosis or pulmonary embolism (blood clots) – rare, but serious risks.
Risk Mitigation
Adherence to preoperative and postoperative instructions, thorough health assessments, and choosing a qualified, board-certified plastic surgeon help minimize complications and promote safe outcomes.
Associated Costs
Understanding Gynecomastia Surgery Costs
The price of gynecomastia surgery can differ based on factors including surgeon’s experience, geographic region, facility fees, and the complexity of the procedure required. During your consultation, discuss with your surgeon an estimate tailored to your specific needs.
Insurance Coverage
Although gynecomastia surgery is often viewed as elective cosmetic surgery, in certain cases insurance may provide coverage if medically justified. It is advisable to check with your insurance provider to determine your eligibility and coverage options.
Financial Planning
If insurance does not cover your procedure, many clinics and surgeons offer financing plans to assist patients in managing the cost of surgery over time. When selecting a surgeon, prioritize expertise and quality over price to ensure the best results and safety.
The Aesthetic Society emphasizes patient safety and quality with a focus on board-certified plastic surgeons who meet rigorous standards in credentialing, education, and ethical practice.

